Kidney stone
| Kidney stone | |
|---|---|
| Classification and external resources | |
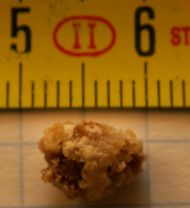 A 8-mm kidney stone. |
|
| ICD-10 | N20.0 |
| ICD-9 | 592.0 |
| DiseasesDB | 11346 |
| MedlinePlus | 000458 |
| eMedicine | med/1600 |
| MeSH | D007669 |
Kidney stones (ureterolithiasis) result from stones or renal calculi (from Latin ren, renes, "kidney" and calculi, "pebbles"[1]) in the ureter. The stones are solid concretions or calculi (crystal aggregations) formed in the kidneys from dissolved urinary minerals. Nephrolithiasis (from Greek νεφρός (nephros, "kidney") and λιθoς (lithos, "stone")) refers to the condition of having kidney stones. Urolithiasis refers to the condition of having calculi in the urinary tract (which also includes the kidneys), which may form or pass into the urinary bladder. Ureterolithiasis is the condition of having a calculus in the ureter, the tube connecting the kidneys and the bladder. The term bladder stones usually applies to urolithiasis of the bladder in non-human animals such as dogs and cats.
Kidney stones typically leave the body by passage in the urine stream, and many stones are formed and passed without causing symptoms. If stones grow to sufficient size before passage on the order of at least 2-3 millimeters they can cause obstruction of the ureter. The resulting obstruction causes dilation or stretching of the upper ureter and renal pelvis (the part of the kidney where the urine collects before entering the ureter) as well as muscle spasm of the ureter, trying to move the stone. This leads to pain, most commonly felt in the flank, lower abdomen and groin (a condition called renal colic). Renal colic can be associated with nausea and vomiting. There can be blood in the urine, visible with the naked eye or under the microscope (macroscopic or microscopic hematuria) due to damage to the lining of the urinary tract.
There are several types of kidney stones based on the type of crystals of which they consist. The majority are calcium oxalate stones, followed by calcium phosphate stones. More rarely, struvite stones are produced by urea-splitting bacteria in people with urinary tract infections, and people with certain metabolic abnormalities may produce uric acid stones or cystine stones.
The diagnosis of a kidney stone can be confirmed by radiological studies and or ultrasound examination; urine tests and blood tests are also commonly performed. When a stone causes no symptoms, watchful waiting is a valid option. In other cases, pain control is the first measure, using for example non-steroidal anti-inflammatory drugs or opioids. Using soundwaves, some stones can be shattered into smaller fragments (this is called extracorporeal shock wave lithotripsy). Sometimes a procedure is required, which can be through a tube into the urethra, bladder and ureter (ureteroscopy), or a keyhole or open surgical approach from the kidney's side. Sometimes, a tube may be left in the ureter (a ureteric stent) to prevent the recurrence of pain. Preventive and structive measures are often advised such as drinking sufficient amounts of water and milk although the effect of many dietary interventions has not been rigorously studied.
Contents |
Signs and symptoms
Symptoms of kidney stones include:[2][3]

- Colicky pain: "loin to groin". Often described as "the worst pain [...] ever experienced". This can also occur in the lower back.[4]
- Nausea/vomiting: embryological link with intestine– stimulates the vomiting center.
- Hematuria: blood in the urine, due to minor damage to inside wall of kidney, ureter and/or urethra.
- Pyuria: pus in the urine.
- Dysuria: burning on urination when passing stones (rare). More typical of infection.
- Oliguria: reduced urinary volume caused by obstruction of the bladder or urethra by stone, or extremely rarely, simultaneous obstruction of both ureters by a stone.
- Postrenal azotemia: the blockage of urine flow through a ureter.[5]
- Hydronephrosis:[6] the distension and dilation of the renal pelvis and calyces.
Causes
Kidney stones or calcium oxalate crystals in kidney can be due to underlying metabolic conditions, such as renal tubular acidosis,[7] Dent's disease,[8] hyperparathyroidism,[9] primary hyperoxaluria[10] and medullary sponge kidney.[11] Kidney stones are also more common in patients with Crohn's disease.[12] Patients with recurrent kidney stones should be screened for these disorders. This is typically done with a 24 hour urine collection that is chemically analyzed for deficiencies and excesses that promote stone formation.[13]
There has been some evidence that water fluoridation may increase the risk of kidney stone formation. In one study, patients with symptoms of skeletal fluorosis were 4.6 times as likely to develop kidney stones.[14]
A 1998 paper in the Archives of Internal Medicine examined the sources of a widely-held belief in the medical community that vitamin C can cause kidney stones, and found it to be based on several circular references, ultimately attributing the belief to a wider pattern of skepticism regarding efficacy of vitamin supplements.[15] A more recent study suggested a causal relationship may exist, but it was not conclusive.[16]
The American Urological Association has projected that increasing global temperatures will lead to greater future prevalence of kidney stones, notably by expanding the "kidney stone belt" of the southern United States.[17] Astronauts seem to show a higher risk of developing kidney stones during or after long duration space flights.[18]
Calcium oxalate stones
The most common type of kidney stone is composed of calcium oxalate crystals, occurring in about 80% of cases,[7] and the factors that promote the precipitation of crystals in the urine are associated with the development of these stones.
Common sense has long held that consumption of too much calcium could promote the development of calcium kidney stones. However, current evidence suggests that the consumption of low-calcium diets is actually associated with a higher overall risk for the development of kidney stones.[2] This is perhaps related to the role of calcium in binding ingested oxalate in the gastrointestinal tract. As the amount of calcium intake decreases, the amount of oxalate available for absorption into the bloodstream increases; this oxalate is then excreted in greater amounts into the urine by the kidneys. In the urine, oxalate is a very strong promoter of calcium oxalate precipitation, about 15 times stronger than calcium.
Uric acid (urate)
About 5–10% of all stones are formed from uric acid.[7] Uric acid stones form in association with conditions that cause hyperuricosuria with or without high blood serum uric acid levels (hyperuricemia); and with acid/base metabolism disorders where the urine is excessively acidic (low pH) resulting in uric acid precipitation. A diagnosis of uric acid nephrolithiasis is supported if there is a radiolucent stone, a persistent undue urine acidity, and uric acid crystals in fresh urine samples.[19]
Other types
Other types of kidney stones are composed of struvite (magnesium, ammonium and phosphate); calcium phosphate; and cystine.
Struvite stones are also known as infection stones, urease or triple-phosphate stones. About 10–15% of urinary calculi consist of struvite stones.[20] The formation of struvite stones is associated with the presence of urea-splitting bacteria,[21] most commonly Proteus mirabilis (but also Klebsiella, Serratia, Providencia species). These organisms are capable of splitting urea into ammonia, decreasing the acidity of the urine and resulting in favorable conditions for the formation of struvite stones. Struvite stones are always associated with urinary tract infections.[20]
The formation of calcium phosphate stones is associated with conditions such as hyperparathyroidism and renal tubular acidosis.
Formation of cystine stones is uniquely associated with people suffering from cystinuria, who accumulate cystine in their urine. Cystinuria can be caused by Fanconi's syndrome.
Urolithiasis has also been noted to occur in the setting of therapeutic drug use, with crystals of drug forming within the renal tract in some patients currently being treated with Indinavir, Sulfadiazine or Triamterene.
Diagnosis
Clinical diagnosis is usually made on the basis of the location and severity of the pain, which is typically colicky in nature (comes and goes in spasmodic waves). Pain in the back occurs when calculi produce an obstruction in the kidney.[3]
Imaging is used to confirm the diagnosis and a number of other tests can be undertaken to help establish both the possible cause and consequences of the stone.
X-rays
The relatively dense calcium renders these stones radio-opaque and they can be detected by a traditional X-ray of the abdomen that includes the kidneys, ureters and bladder—KUB.[22] This may be followed by an IVP (intravenous pyelogram—intravenous urogram (IVU) is the same test by another name) which requires about 50 ml of a special dye to be injected into the bloodstream that is excreted by the kidneys and by its density helps outline any stone on a repeated X-ray. These can also be detected by a retrograde pyelogram where similar "dye" is injected directly into the ureteral opening in the bladder by a surgeon, usually a urologist.
About 10% of stones do not have enough calcium to be seen on standard X-rays (radiolucent stones).
Computed tomography
Computed tomography without contrast is considered the gold standard diagnostic test for the detection of kidney stones. All stones are detectable by CT except very rare stones composed of certain drug residues in the urine.[22] If positive for stones, a single standard X-ray of the abdomen (KUB) is recommended. This gives a clearer idea of the exact size and shape of the stone as well as its surgical orientation. Further, it makes it simple to follow the progress of the stone by doing another X-ray in the future.
Drawbacks of CT scans include radiation exposure and cost.
Ultrasound
Ultrasound imaging is useful as it gives details about the presence of hydronephrosis (swelling of the kidney—suggesting the stone is blocking the outflow of urine).[22] It can also be used to detect stones during pregnancy when x-rays or CT are discouraged. Radiolucent stones may show up on ultrasound however they are also typically seen on CT scans.
Some recommend that US be used as the primary diagnostic technique with CT being reserved for those with negative US result and continued suspicion of a kidney stone. This is due to its lesser cost and avoidance of radiation.[23]
Other
Other investigations typically carried out include:[22]
- Microscopic study of urine, which may show proteins, red blood cells, bacteria, cellular casts and crystals.
- Culture of a urine sample to exclude urine infection (either as a differential cause of the patient's pain, or secondary to the presence of a stone)
- Blood tests: Full blood count for the presence of a raised white cell count (Neutrophilia) suggestive of infection, a check of renal function and to look for abnormally high blood calcium blood levels (hypercalcaemia).
- 24 hour urine collection to measure total daily urinary volume, magnesium, sodium, uric acid, calcium, citrate, oxalate and phosphate.
- Catching of passed stones at home (usually by urinating through a tea strainer or stonescreen) for later examination and evaluation by a doctor.[24][25]
Gallery
 Staghorn calculus |
Multiple kidney stones composed of uric acid and a small amount of calcium oxalate. |
 Star-shaped bladder urolith on an X-ray of the pelvis. |
 Bilateral kidney stones on abdominal X-ray. Not to be confused with phleboliths seen in the pelvis. |
|
CT of abdomen without contrast showing right proximal ureteric stone causing mild obstruction and hydronephrosis (marked by an arrow). |
 A kidney stone at the tip of an ultrasonic instrument. |
 Three-dimensional reconstructed CT scan image of a ureteral stent in the left kidney (indicated by yellow arrow). There is a kidney stone in the pyelum of the lower pole of the kidney (highest red arrow) and one in the ureter beside the stent (lower red arrow). |
Prevention
Preventive strategies include dietary modifications and sometimes also taking drugs with the goal of reducing excretory load on the kidneys:[2][26]
- Drinking enough water to make 2 to 2.5 liters of urine per day.
- A diet low in protein, nitrogen and sodium intake .
- Restriction of oxalate-rich foods, such as chocolate, nuts, soybeans,[27] rhubarb and spinach,[28] plus maintenance of an adequate intake of dietary calcium. There is equivocal evidence that calcium supplements increase the risk of stone formation, though calcium citrate appears to carry the lowest, if any, risk.
- Taking drugs such as thiazides, potassium citrate, magnesium citrate and allopurinol, depending on the cause of stone formation.
- Some fruit juices, such as orange, blackcurrant, and cranberry, may be useful for lowering the risk factors for specific types of stones. Orange juice may help prevent calcium oxalate stone formation, black currant may help prevent uric acid stones, and cranberry may help with UTI-caused stones.[29][30]
- Limit intake of caffeinated beverages, such as coffee.[31][32]
- Avoidance of cola beverages.[33][34]
- Avoiding large doses of vitamin C.[35]
- On the Indian subcontinent, there is a popular cultural belief that spinach should not be cooked along with tomatoes, since spinach is rich in calcium and oxalates, and reacts with the chemicals in tomatoes, causing deposits in those prone to kidney stone formation. However, this theory is not scientifically proven and is controversial.
For those patients interested in optimizing their kidney stone prevention options, a 24 hour urine test can be a useful diagnostic.
Restricting oxalate consumption
Calcium plays a vital role in body chemistry so limiting calcium may be unhealthy. Since calcium in the intestinal tract will bind with available oxalate, thereby preventing its absorption into the blood stream, some nephrologists and urologists recommend chewing calcium tablets during meals containing oxalate foods. However, a more reliable approach is to restrict the intake of food that is high in oxalate (see oxalate for a list). This is only helpful in those patients who are absorbing excess oxalate which is a minority of patients as most oxalate excreted in the urine is actually made by the liver.
Diuretics
Although it has been claimed that the diuretic effects of alcohol can result in dehydration, which is important for kidney stone sufferers to avoid, there are no conclusive data demonstrating any cause and effect regarding kidney stones. However, some have theorized that frequent and binge drinkers create situations that set up dehydration: alcohol consumption, hangovers, and poor sleep and stress habits. In this view, it is not the alcohol that creates a kidney stone but it is the alcohol drinker's associated behavior that sets it up.[36]
One of the recognized medical therapies for prevention of stones is thiazides, a class of drugs usually thought of as diuretics. These drugs prevent calcium stones through an effect independent of their diuretic properties: they reduce urinary calcium excretion. Nonetheless, their diuretic property does not preclude their efficacy as stone preventive. Sodium restriction is necessary for clinical effect of thiazides, as sodium excess promotes calcium excretion. Thiazides work best for renal leak hypercalciuria - a condition in which the high urinary calcium levels are from a primary kidney defect. They work well initially for absorptive hypercalciuria - a condition in which high urinary calcium is a result of excess absorption from the GI tract. With this condition they lose effectiveness over time, typically around 2 years, and patients need a period off treatment to regain effectiveness. Thiazides will cause hypokalemia and reduced urinary citrate levels so should be given with supplements for each, usually as a potassium citrate preparation.
Allopurinol
Allopurinol (Zyloprim) is another drug with proven benefits in some calcium kidney stone formers. Allopurinol interferes with the liver's production of uric acid. Hyperuricosuria, too much uric acid in the urine, is a risk factor for calcium stones. Allopurinol reduces calcium stone formation in such patients. The drug is also used in patients with gout or hyperuricemia.[37] However, hyperuricemia is not the critical feature of uric acid stones, which can occur in the presence of hypouricemia. Uric acid stones are more often caused by a combination of high urine uric acid and low urine pH.[38] Even relatively high uric acid excretion will not be associated with uric acid stone formation if the urine pH is alkaline. Therefore prevention of uric acid stones relies on alkalinization of the urine with citrate (in the form of Shohl's solution (sodium citrate), sodium bicarbonate, potassium citrate, potassium bicarbonate or acetazolamide, a carbonic anhydrase inhibitor).
Allopurinol is reserved for patients in whom alkalinization is difficult. For patients with increased uric acid levels and calcium stones, allopurinol is one of the few treatments that has been shown in double-blinded placebo controlled studies to actually reduce kidney stone recurrences. Dosage is adjusted to maintain a reduced urinary excretion of uric acid. Serum uric acid level at or below 6 mg/dL is often the goal of the drug's use in patients with gout or hyperuricemia.
Decreased-protein diet
A high-protein diet might be partially to blame . Protein from meat and other animal products is broken down into acids, including uric acid. The most available alkaline base to balance the acid from protein is calcium phosphate (hydroxyapatite) from the bones (buffering). The kidney filters the liberated calcium which may then form insoluble crystals (i.e., stones) in urine with available oxalate (partly from metabolic processes, partly from diet) or phosphate ions, depending on conditions . High protein intake is therefore associated with decreased bone density as well as stones. The acid load is associated with decreased urinary citrate excretion ; citrate competes with oxalate for calcium and can thereby prevent stones.
In addition to increased fluid intake, one of the simplest fixes is to moderate animal protein consumption . However, despite epidemiologic data showing that greater protein intake is associated with more stones, randomized controlled trials of protein restriction have not shown reduced stone prevalence . In this regard, it is not just dietary calcium per se that may cause stone formation, but rather the leaching of bone calcium . Some diseases (e.g., distal renal tubular acidosis) which cause a chronically acidic state also decrease urinary citrate levels; since citrates are normally present as potent inhibitors of stone formation, these patients are prone to frequent stone formation .
Other modifications
Potassium citrate is also used in kidney stone prevention. This is available as both a tablet and liquid preparation. The medication increases urinary pH (makes it more alkaline), as well as increases the urinary citrate level, which helps reduce calcium oxalate crystal aggregation. Optimal 24 hour urine levels of citrate are thought to be over 320 mg/liter of urine or over 600 mg per day. There are urinary dipsticks available that allow patients to monitor and measure urinary pH so patients can optimize their urinary citrate level.
Though caffeine does acutely increase urinary calcium excretion, several independent epidemiologic studies have shown that coffee intake overall is protective against the formation of stones.[39]
Measurements of food oxalate content have been difficult and issues remain about the proportion of oxalate that is bio-available, versus a proportion that is not absorbed by the intestine. Oxalate-rich foods are usually restricted to some degree, particularly in patients with high urinary oxalate levels, but no randomized controlled trial of oxalate restriction has been performed to test that hypotheses.
Calgranulin
Crystallization of calcium oxalate (CaOx) appears to be reduced by molecules in the urine that retard the formation, growth, aggregation, and renal cell adherence of calcium oxalate. By purifying urine using salt precipitation, preparative isoelectric focusing, and sizing chromatography, some researchers have found that the molecule calgranulin is able to inhibit calcium oxalate crystal growth.[40] Calgranulin is a protein formed in the kidney. Given the large amounts of calcium oxalate in the urine, and considering its potency, calgranulin could become an important contribution to the normal urinary inhibition of crystal growth and aggregation. If so, it will be an important tool in the renal defense against kidney stones.
Medical management
There has been some debate regarding the usefulness of medical management overall in the treatment of stone forming patients. Despite this debate, it is clear that repeat stone formers do benefit from more intense management, including proper hydration and use of certain medications. Additionally, it is also clear that careful surveillance is required in order to maximize the clinical course for patients who are unlucky enough to be stone formers.[41][42]
Management
Conservative
About 90% of stones 4 mm or less in size usually will pass spontaneously, however 99% of stones larger than 6 mm will require some form of intervention.[43] There are various measures that can be used to encourage the passage of a stone. These can include increased hydration, medication for treating infection and reducing pain, and diuretics to encourage urine flow and prevent further stone formation. Caution should be exercised in eating certain foods, such as starfruit, with high concentrations of oxalate which may precipitate acute renal failure in patients with chronic renal disease.[44]
In most cases, a smaller stone that is not symptomatic is often given up to four weeks[2] to move or pass before consideration is given to any surgical intervention as it has been found that waiting longer tends to lead to additional complications. Immediate surgery may be required in certain situations such as in people with only one working kidney, bilateral obstructing stones, intractable pain or in the presence of an infected kidney blocked by a stone which can cause sepsis.
Straining the urine allows collection of the stone when it passes. Analysis can help establish preventative options.
Analgesia
Management of pain often requires intravenous administration of NSAIDS or opioids in an emergency room setting. Orally-administered medications are often effective for less severe discomfort (NSAIDs or opioids). Intravenous acetaminophen also appears to be effective.[45]
After treatment, the pain may return if the stone moves but re-obstructs in another location.
Alpha adrenergic blockers
Alpha adrenergic blockers such as tamsulosin (Flomax) may increase the spontaneous passage of the stone by 30%. Recent studies have, however, questioned this claim, finding no benefit from these medications.[46]
Urologic interventions
Most kidney stones do not require surgery and will pass on their own. Surgery is necessary when the pain is persistent and severe, in renal failure and when there is a kidney infection. It may also be advisable if the stone fails to pass or move after 30 days. Finding a significant stone before it passes into the ureter allows physicians to fragment it surgically before it causes any severe problems. In most of these cases, non-invasive extracorporeal shock wave lithotripsy (ESWL) will be used. Otherwise some form of invasive procedure is required; with approaches including ureteroscopic fragmentation (or simple basket extraction if feasible) using laser, ultrasonic or mechanical (pneumatic, shock-wave) forms of energy to fragment the larger stones. Percutaneous nephrolithotomy or rarely open surgery may ultimately be necessary for large or complicated stones or stones which fail other less invasive attempts at treatment.
A single retrospective study in the USA, at the Mayo Clinic, has suggested that lithotripsy may increase subsequent incidence of diabetes and hypertension,[47] but it has not been felt warranted to change clinical practice at the clinic.[48] The study reflects early experience with the original lithotripsy machine which had a very large blast path, much larger than what is used on modern machines. Further study is believed necessary to determine how much risk this treatment actually has using modern machines and treatment regimens.
More common complications related to ESWL are bleeding, pain related to passage of stone fragments, failure to fragment the stone, and the possible requirement for additional or alternative interventions.
Ureteral (double-J) stents
One modern medical technique uses a ureteral stent (a small tube between the bladder and the inside of the kidney) to provide immediate relief of a blocked kidney. This is especially useful in saving a failing kidney due to swelling and infection from the stone. Ureteral stents vary in length and width but most have the same shape usually called a "double-J" or "double pigtail", because of the curl at both ends. They are designed to allow urine to drain around any stone or obstruction. They can be retained for some length of time as infections recede and as stones are dissolved or fragmented with ESWL or other treatment. The stents will gently dilate or stretch the ureters which can facilitate instrumentation and they will also provide a clear landmark to help surgeons see the stones on x-ray. Most stents can be removed easily during a final office visit. Discomfort levels from stents typically range from minimal associated pain to moderate discomfort. However, it isn't uncommon for patients to experience severe discomfort too, especially upon removal of said stent.
The use of ureteral stents is of particular significance in the treatment of ureteral stones. Their use, non use, and circumstances peculiar to stents should be well understood in order to maximize the benefits.[49]
Epidemiology
Within the United States, about 10–15% of adults will be diagnosed with a kidney stone,[50] and the total cost for treating this condition was US$2 billion in 2003.[22] The incidence rate increases to 20–25% in the Middle East, because of increased risk of dehydration in hot climates. (The typical Arabian diet is also 50% lower in calcium and 250% higher in oxalates compared to Western diets, increasing the net risk.)[51] Recurrence rates are estimated at about 10% per year, totalling 50% over a 5–10 year period and 75% over 20 years.[7] Men are affected approximately 4 times more often than women. Recent evidence has shown an increase in pediatric cases.[52]
History
The existence of kidney stones has been recorded since the beginning of civilization, and lithotomy for the removal of stones is one of the earliest known surgical procedures.[53] In 1901, a stone was discovered in the pelvis of an ancient Egyptian mummy, and was dated to 4,800 BC. Medical text from ancient Mesopotamia, India, China, Persia, Greece and Rome all mentioned calculous disease. Part of the Hippocratic oath contains an admonition about the dangers of operating on the bladder for stones. The Roman medical treatise De Medicina by Cornelius Celsus contained a description of lithotomy, and this work served as the basis for this procedure up until the 18th century.[54]
New techniques in lithotomy began to emerge starting in 1520, but the operation remained risky. It was only after Henry Jacob Bigelow popularized the technique of litholapaxy in 1878 that the mortality rate dropped from about 24% down to 2.4%. However, other treatment techniques were developed that continued to produce a high level of mortality, especially among inexperienced urologists.[54][55] In 1980, Dornier MedTech introduced extracorporeal shock wave lithotripsy for breaking up stones via acoustical pulses, and this technique has come into widespread use.[56]
See also
- Nephrology
- Urinary retention
- Urology
- Retrograde pyelogram
- Cystinuria
- Intravenous pyelogram
- Kidney stone sufferers
References
- ↑ Collins, C. Edward (2005). A Short Course in Medical Terminology. Lippincott Williams & Wilkins. ISBN 0781747678.
- ↑ 2.0 2.1 2.2 2.3 Parmar, Malvinder S. (2004). "Kidney stones". British Medical Journal 328 (7453): 1420–1424. doi:10.1136/bmj.328.7453.1420. PMID 15191979.
- ↑ 3.0 3.1 Weaver, S. H.; Jenkins, P. et al. (2002). "Chapter 14: Renal and Urological Care". Illustrated Manual of Nursing Practice (3rd ed.). Lippincott Williams & Wilkins. ISBN 1582550824.
- ↑ Mayo Clinic (2008). "Kidney Stone Channel". U.S. News & World Report. http://health.usnews.com/usnews/health/pain/kidneystone/kidneystone.about.htm. Retrieved 2008-04-23.
- ↑ Goljan, Edward F. (2007). Rapid Review Pathology (2nd ed.). Mosby. pp. 397. ISBN 0-323-04414-X.
- ↑ Kumar, Vinay; Fausto, Nelson; Fausto, Nelso; Robbins, Stanley L.; Abbas, Abul K.; Cotran, Ramzi S. (2005). Robbins and Cotran Pathologic Basis of Disease (7th ed.). Philadelphia, Pa.: Elsevier Saunders. pp. 1012. ISBN 0-7216-0187-1.
- ↑ 7.0 7.1 7.2 7.3 Moe, Orson W. (2006). "Kidney stones: pathophysiology and medical management". The Lancet 367 (9507): 333–344. doi:10.1016/S0140-6736(06)68071-9.
- ↑ Lloyd SE, Pearce SHS; Fisher SE; Steinmeyer K, Schwappach B, Scheinman SJ, Harding B, Bolino A, Devoto M, Goodyer P, Rigden SPA, Wrong O, Jentsch TJ, Craig IW, Thakker RV (1996). "A common molecular basis for three inherited kidney stone diseases". Nature 379 (6564): 445–449. doi:10.1038/379445a0. PMID 8559248.
- ↑ "Hyperparathyroidism". National Endocrine and Metabolic Diseases Information Service. National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. May 2006. http://www.endocrine.niddk.nih.gov/pubs/hyper/hyper.htm#symptoms.
- ↑ Hoppe B, Langman CB (October 2003). "A United States survey on diagnosis, treatment, and outcome of primary hyperoxaluria". Pediatric Nephrology 18 (10): 986–991. doi:10.1007/s00467-003-1234-x. PMID 12920626.
- ↑ Ginalski JM, Portmann L, Jaeger P (August 1, 1991). "Does medullary sponge kidney cause nephrolithiasis?". American Journal of Roentgenology 156 (4): 872–3. PMID 2115256. http://www.ajronline.org/cgi/content/abstract/155/2/299. Retrieved 2008-03-12.
- ↑ Böhles H, Beifuss OJ, Brandl U, Pichl J, Akçetin Z, Demling L (February 1, 1988). "Urinary factors of kidney stone formation in patients with Crohn's disease". Klinische Wochenschr 66 (3): 87–91. PMID 3352194.
- ↑ Marshall Cavendish Corporation (2007). Diseases and Disorders, volume 2. Marshall Cavendish. p. 491. ISBN 0761477721.
- ↑ National Research Council (2002). Fluoride in Drinking Water: A Scientific Review of EPA's Standard. New York: National Academies Press. ISBN 030910128X.
- ↑ Goodwin JS, Mangum MR (November 9, 1998). "Battling quackery: attitudes about micronutrient supplements in American academic medicine". Archives of Internal Medicine 158 (20): 2187–91. doi:10.1001/archinte.158.20.2187. PMID 9818798. http://archinte.ama-assn.org/cgi/pmidlookup?view=long&pmid=9818798. Retrieved 2010-03-06. Note: login required
- ↑ Massey LK, Liebman M, Kynast-Gales SA (2005). "Ascorbate increases human oxaluria and kidney stone risk" (PDF). Journal of Nutrition 135 (7): 1673–7. PMID 15987848. http://jn.nutrition.org/cgi/reprint/135/7/1673.pdf.
- ↑ "Global Warming May Lead To Increase In Kidney Stones Disease". ScienceDaily. May 15, 2008. http://www.sciencedaily.com/releases/2008/05/080515072740.htm. Retrieved 2010-03-06.
- ↑ Ciftçioglu N, Haddad RS, Golden DC, Morrison DR, McKay DS (February 2005). "A potential cause for kidney stone formation during space flights: enhanced growth of nanobacteria in microgravity". Kidney International 67 (2): 483–91. doi:10.1111/j.1523-1755.2005.67105.x. PMID 15673296.
- ↑ Halabe A, Sperling O (1994). "Uric acid nephrolithiasis". Mineral and electrolyte metabolism 20 (6): 424–31. PMID 7783706.
- ↑ 20.0 20.1 Jennette JC, Heptinstall RH (2007). J. Charles Jennette, Jean L. Olson et al.. ed. Heptinstall's pathology of the kidney. 1 (6th ed.). Lippincott Williams & Wilkins. p. 1063. ISBN 0781747503.
- ↑ Rodman JS (1999). "Struvite Stones". Proceedings of the International ASTIF Meeting, New Frontiers in Renal Stone Disease. 81. Fiuggi (Rome), Italy. http://content.karger.com/ProdukteDB/produkte.asp?Aktion=ShowAbstract&ArtikelNr=000046299&Ausgabe=226754&ProduktNr=223854. Retrieved 2010-02-06.
- ↑ 22.0 22.1 22.2 22.3 22.4 Pietrow, Paul K.; Karellas, Michael E. (2006). "Medical Management of Common Urinary Calculi". American Family Physician 74 (1): 86–94. http://www.aafp.org/afp/20060701/86.html. Retrieved 2008-05-20.
- ↑ "BestBets: ultrasound vs CT scan for detecting calculi". http://www.bestbets.org/bets/bet.php?id=964.
- ↑ Anonymous (October 2007). "How are kidney stones treated?". Kidney Stones in Adults. National Institute of Diabetes and Digestive and Kidney Diseases. http://kidney.niddk.nih.gov/kudiseases/pubs/stonesadults/#treatment. Retrieved 2008-05-20.
- ↑ Anonymous (2008). "Kidney Stones". Cape Fear Valley Medical Center. http://www.health-news-and-information.com/4cfvhs/libv/i24.shtml. Retrieved 2008-05-20.
- ↑ Goldfarb, David S.; Coe, Fredric L. (November 15, 1999). "Prevention of recurrent nephrolithiasis". American Family Physician 60 (8): 2269–76. PMID 10593318. http://www.aafp.org/afp/991115ap/2269.html.
- ↑ Hassell, Beverly (2001-08-28). "Too much soy could lead to kidney stones". EurekAlert. http://www.eurekalert.org/pub_releases/2001-08/acs-tms082801.php. Retrieved 2008-06-28.
- ↑ Prenen, J. A.; Boer P.; Dorhout Mees, E. J. (1984). "Absorption kinetics of oxalate from oxalate-rich food in man". The American Journal of Clinical Nutrition 40 (5): 1007–1010. PMID 6496379. http://www.ajcn.org/cgi/content/abstract/40/5/1007. Retrieved 2010-02-26.
- ↑ Kelera,, T.; Jansen, B.; Hesse, A. (2002). "Effect of blackcurrant-, cranberry- and plum juice consumption on risk factors associated with kidney stone formation". European Journal of Clinical Nutrition 56 (10): 1020–1023. doi:10.1038/sj.ejcn.1601442. PMID 12373623. http://www.nature.com/ejcn/journal/v56/n10/abs/1601442a.html. Retrieved 2008-05-12.
- ↑ Odvina, Clarita V. (2006). "Comparative Value of Orange Juice versus Lemonade in Reducing Stone-Forming Risk". Clinical Journal of the American Society of Nephrology 1 (6): 1269–74. doi:10.2215/CJN.00800306. PMID 17699358. http://cjasn.asnjournals.org/cgi/content/abstract/1/6/1269. Retrieved 2008-05-12.
- ↑ "Watch your caffeine intake if you are prone to kidney stones". http://www.medicalnewstoday.com/articles/12937.php. Retrieved 2010-02-26.
- ↑ Massey, Linda K.; Sutton, Roger A. L. (August 2004). "Acute Caffeine Effects on Urine Composition and Calcium Kidney Stone Risk in Calcium Stone Formers". The Journal of Urology 172 (2): 555–558. doi:10.1097/01.ju.0000129413.87024.5c. PMID 15247728.
- ↑ O'Connor, Anahad (January 22, 2008). "The Claim: Too Much Cola Can Cause Kidney Problems". The New York Times. http://www.nytimes.com/2008/01/22/health/nutrition/22real.html?_r=1&oref=slogin. Retrieved 2008-04-23.
- ↑ Saldana, Tina M.; Basso, Olga; Darden, Rebecca; Sandler, Dale P. (2007). "Carbonated Beverages and Chronic Kidney Disease". Epidemiology 18 (4): 501–506. doi:10.1097/EDE.0b013e3180646338. PMID 17525693. http://www.epidem.com/pt/re/epidemiology/abstract.00001648-200707000-00017.htm. Retrieved 2008-05-12.
- ↑ Taylor, Eric N. coauthors=Stampfer, Meir J.; Curhan, Gary C.; Stampfer, MJ; Curhan, GC (2004). "Dietary Factors and the Risk of Incident Kidney Stones in Men: New Insights after 14 Years of Follow-up". Journal of the American Society of Nephrology 15 (6): 3225–3232. doi:10.1097/01.ASN.0000146012.44570.20. PMID 15579526.
- ↑ Rodman, John S.; Seidman, Cynthia (1996). No More Kidney Stones. Wiley. ISBN 0471125873.
- ↑ Cameron JS, Simmonds HA (June 1987). "Use and abuse of allopurinol". British Medical Journal 294 (6586): 1504–5. doi:10.1136/bmj.294.6586.1504. PMID 3607420.
- ↑ Martín Hernández E, Aparicio López C, Alvarez Calatayud G, García Herrera MA (September 2001). "[Vesical uric acid lithiasis in a child with renal hypouricemia"] (in Spanish). Anales Españoles De Pediatría 55 (3): 273–6. PMID 11676906. http://db.doyma.es/cgi-bin/wdbcgi.exe/doyma/mrevista.pubmed_full?inctrl=05ZI0103&rev=37&vol=55&num=3&pag=273.
- ↑ Curhan GC, Willett WC, Rimm EB, Spiegelman D, Stampfer MJ (1 February 1996). "Prospective Study of Beverage Use and the Risk of Kidney Stones". Am Jour Epidemiology 143 (3): 240–247. PMID 8561157. http://aje.oxfordjournals.org/cgi/content/abstract/143/3/240.
- ↑ Pillay, Sokalingum N.; Asplin, John R.; Coe, Fredric L. (August 1, 1998). "Evidence that calgranulin is produced by kidney cells and is an inhibitor of calcium oxalate crystallization". American Journal of Physiology - Renal Physiology 275 (2): F255–F261. PMID 9691016. http://ajprenal.physiology.org/cgi/content/abstract/275/2/F255. Retrieved 2008-04-23.
- ↑ Preminger GM, Macaluso JN (May 1996). Is renal stone medical management underused? Physician’s Weekly. 13.
- ↑ Macaluso JN (November 1996). "Management of stone disease--bearing the burden". The Journal of Urology 156 (5): 1579–80. doi:10.1016/S0022-5347(01)65452-1. PMID 8863542.
- ↑ Reilly, Robert F. (2005). Nephrology in 30 Days. UNC Press. p. 195. ISBN 1882886208.
- ↑ Chang JM, Hwang SJ, Kuo HT, et al. (February 2000). "Fatal outcome after ingestion of star fruit (Averrhoa carambola) in uremic patients". American Journal of Kidney Diseases 35 (2): 189–93. doi:10.1016/S0272-6386(00)70325-8. PMID 10676715.
- ↑ Bektas F, Eken C, Karadeniz O, Goksu E, Cubuk M, Cete Y (October 2009). "Intravenous paracetamol or morphine for the treatment of renal colic: a randomized, placebo-controlled trial". Ann Emerg Med 54 (4): 568–74. doi:10.1016/j.annemergmed.2009.06.501. PMID 19647342.
- ↑ Ferre RM, Wasielewski JN, Strout TD, Perron AD (September 2009). "Tamsulosin for ureteral stones in the emergency department: a randomized, controlled trial". Ann Emerg Med 54 (3): 432–9, 439.e1–2. doi:10.1016/j.annemergmed.2008.12.026. PMID 19200622.
- ↑ Krambeck, A.; Gettman, M.; Rohlinger, A.; Lohse, C.; Patterson, D.; Segura, J. (2006). "Diabetes mellitus and hypertension associated with shock wave lithotripsy of renal and proximal ureteral stones at 19 years of followup". The Journal of Urology 175 (5): 1742–7. doi:10.1016/S0022-5347(05)00989-4. PMID 16600747.
- ↑ Edelson, Ed (April 12, 2006). "Kidney Stone Shock Wave Treatment Boosts Diabetes, Hypertension Risk - Study suggests link, but doctors say it's too early to abandon this therapy". HealthFinder (National Health Information Center). http://www.medicineonline.com/news/10/8269/Kidney-Stone-Shock-Wave-Treatment-Boosts-Diabetes-Hypertension-Risk.html. Retrieved 2008-05-03.
- ↑ Macaluso JN: Ureteral Stents: Usage Before, During and After Stone Treatment. Problems in Urology, Vol 7 #4, 590 - 600, October-December 1993
- ↑ Stamatelou, Kiriaki K.; Francis, Mildred E.; Jones, Camille A; Nyberg Jr., Leroy M.; Curhan, Gary C. (2003). "Time trends in reported prevalence of kidney stones in the United States: 1976–1994". Kidney International 63 (5): 1817–1823. doi:10.1046/j.1523-1755.2003.00917.x. PMID 12675858.
- ↑ Potts, Jeannette M. (2004). Essential Urology: A Guide to Clinical Practice. Humana Press. pp. 129. ISBN 158829109X.
- ↑ Tarkan, Laurie (2008-10-28). "A Rise in Kidney Stones Is Seen in U.S. Children". New York Times. http://www.nytimes.com/2008/10/28/health/28kidn.html.
- ↑ Eknoyan, Garabed (2004). "History of urolithiasis". Clinical Reviews in Bone and Mineral Metabolism 2 (3): 177–185. doi:10.1385/BMM:2:3:177.
- ↑ 54.0 54.1 Shah J, Whitfield HN (May 2002). "Urolithiasis through the ages". BJU International 89 (8): 801–10. doi:10.1046/j.1464-410X.2002.02769.x. PMID 11972501.
- ↑ Basler, Joseph; Ghobriel, Aldo; Talavera, Francisco; Resnick, Martin I.; Wolf, J. Stuart, Jr.; Leslie, Stephen W. (August 10, 2007). "Bladder Stones". WebMD. http://www.emedicine.com/MED/topic2852.htm. Retrieved 2008-05-22.
- ↑ Auge BK, Preminger GM (July 2002). "Update on shock wave lithotripsy technology". Current Opinion in Urology 12 (4): 287–90. doi:10.1097/00042307-200207000-00005. PMID 12072648.
External links
- International Kidney Stone Institute
- National Kidney and Urologic Diseases Information Clearinghouse
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||